Is Your Gut Making You Gain Weight? The Microbiome-Obesity Connection
You eat well, exercise regularly, and still can't shift the weight. It’s a reality many Australian adults struggle with. But the answer might not be in your gym routine or meal plan, it could be living in your gut.
Research now shows that the trillions of bacteria in your digestive system play a direct role in whether you store fat or burn it, and understanding the gut microbiome and obesity connection could be the missing piece in your weight management puzzle.
Key Insights:
Your gut microbiome directly influences how your body stores and burns fat.
An imbalanced gut can trigger inflammation, increase calorie absorption, and disrupt hormones that control hunger and metabolism.
Specific bacterial strains have been linked to obesity, whilst others protect against weight gain.
Restoring gut health through targeted treatment can support sustainable weight loss when diet and exercise alone haven't worked.
What Is the Gut Microbiome and How Does It Affect Weight?
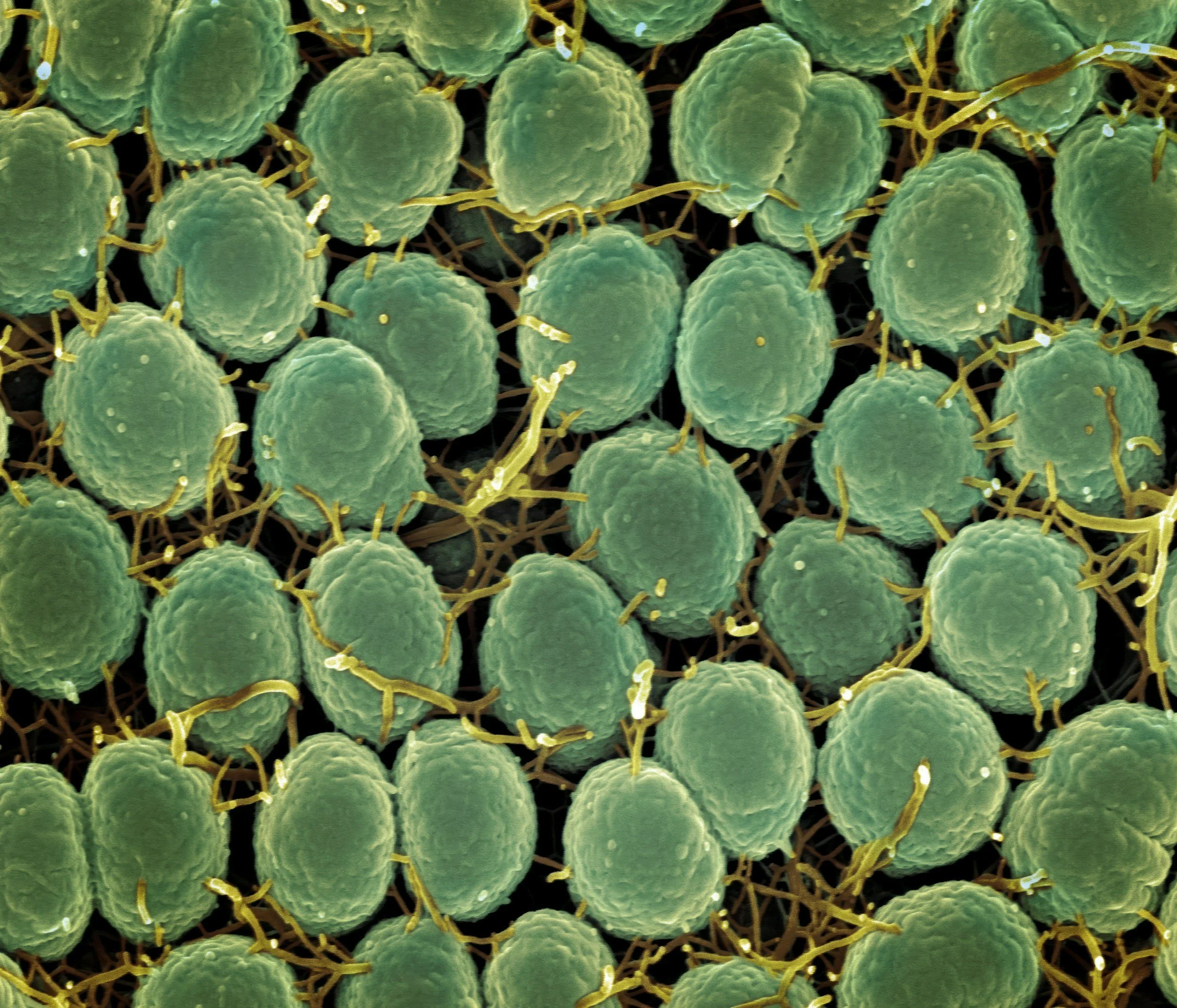
Your gut houses over 100 trillion microorganisms – bacteria, fungi, and other microbes that do far more than digest food. These microbes communicate with your brain, regulate your immune system, and critically, influence how efficiently your body processes nutrients and stores fat.
The link between microbiome and obesity isn't just theoretical. A landmark study published in Nature found that obese individuals have distinctly different gut bacterial profiles compared to lean individuals, with reduced bacterial diversity being a consistent marker.
Here's what happens when your gut microbiome is out of balance:
Increased Calorie Extraction
Certain bacterial strains are exceptionally efficient at breaking down food and extracting every available calorie. When these bacteria dominate your gut, you absorb more energy from the same meal compared to someone with a healthier bacterial balance.
Chronic Low-Grade Inflammation
An unhealthy gut allows bacterial toxins called lipopolysaccharides (LPS) to leak into your bloodstream – a condition known as metabolic endotoxemia. This triggers system-wide inflammation that interferes with insulin signalling and promotes fat storage, particularly around your abdomen.
Disrupted Hunger Hormones
Your gut bacteria produce compounds that directly influence appetite-regulating hormones like ghrelin (which increases hunger) and leptin (which signals fullness). When gut bacteria obesity patterns emerge, these signals become scrambled – you feel hungrier, crave more processed foods, and struggle to feel satisfied after meals.
Which Gut Bacteria Are Linked to Weight Gain?
Not all gut bacteria are created equal when it comes to the gut microbiome and obesity relationship. Scientists have identified specific bacterial groups associated with either weight gain or protection against obesity.
Firmicutes vs Bacteroidetes Ratio: Obese individuals typically have a much higher ratio of Firmicutes to Bacteroidetes – Firmicutes are more efficient at extracting calories from food, while Bacteroidetes help regulate fat storage and reduce inflammation.
Akkermansia Muciniphila: People with higher levels of Akkermansia tend to have healthier metabolic profiles and lower body weight.
Christensenella Minuta: This relatively rare bacterial species is more common in lean individuals and has been shown to prevent weight gain when introduced into animal studies.
Proteobacteria Overgrowth: This bacterial family is associated with gut inflammation and metabolic dysfunction. Elevated Proteobacteria levels correlate with increased visceral fat (the dangerous fat around organs) and insulin resistance.
How Does Gut Health Impact Weight Loss Efforts?
If you've struggled to lose weight despite your best efforts, an imbalanced gut microbiome might be sabotaging your progress. Here's how the gut microbiome and obesity connection plays out in real-world weight loss attempts.
Reduced Metabolic Rate
Gut dysbiosis (an imbalance in gut bacteria) can significantly slow your metabolic rate, meaning you burn fewer calories at rest and during activity. This makes weight loss considerably harder, even when you're eating in a calorie deficit.
Increased Fat Storage Signals
Certain gut bacteria produce short-chain fatty acids (SCFAs) that help regulate fat storage. When beneficial bacteria decline, SCFA production drops, and your body receives stronger signals to store rather than burn fat.
Blood Sugar Dysregulation
An unhealthy gut contributes to insulin resistance, causing your blood sugar to spike and crash throughout the day. This creates intense cravings for refined carbohydrates and sugar, the exact foods that feed harmful gut bacteria, creating a vicious cycle.
Impaired Nutrient Absorption
Even if you're eating nutrient-dense whole foods, gut inflammation can prevent proper absorption of vitamins, minerals, and other compounds your body needs to function optimally. This can leave you feeling fatigued and craving more food as your body searches for missing nutrients.
Can You Change Your Gut Bacteria to Support Weight Loss?
The encouraging news is that your gut microbiome is remarkably adaptable. Unlike your genetics, which are fixed, your gut bacteria can shift significantly within just a few weeks of targeted intervention. Here's what evidence-based approaches look like for addressing gut bacteria obesity treatment.
Dietary diversity matters most: Food diversity is protective against obesity and metabolic disease. Focus on variety: different coloured vegetables, various legumes, nuts, seeds, herbs, and spices all count.
Prebiotic foods feed beneficial bacteria: Foods rich in prebiotic fibre – like onions, garlic, leeks, asparagus, Jerusalem artichokes, and slightly green bananas – selectively feed beneficial gut bacteria whilst starving harmful strains.
Probiotic considerations: Specific probiotic strains like Lactobacillus gasseri and Bifidobacterium lactis have shown promise in clinical trials for supporting weight loss, but individual responses vary significantly.
Polyphenol-rich foods: Compounds found in berries, green tea, dark chocolate, and extra virgin olive oil act as fuel for beneficial bacteria while inhibiting harmful strains.
Stress and sleep management: Prioritising 7-8 hours of quality sleep and implementing stress management techniques helps maintain a healthy gut environment.
When Should You Seek Professional Help?
If you're experiencing ongoing weight gain despite healthy lifestyle habits, or if weight loss efforts consistently fail, it's worth investigating the gut microbiome and obesity connection more deeply.
The relationship between your gut and your weight is bidirectional – obesity affects your microbiome, but your microbiome also influences obesity risk. Breaking this cycle requires a strategic, evidence-based approach that goes beyond conventional weight loss advice.
At Evergreen Doctors, we've seen countless patients finally achieve sustainable weight loss once we addressed their underlying gut health issues. Our practitioners combine comprehensive testing with tailored nutrition plans, targeted supplementation, and lifestyle strategies that address the root causes of weight gain. We've found that when patients understand their gut health and weight loss connection and receive personalised support, they achieve results that previously felt impossible.
Ready to discover what's really happening in your gut? Book a consultation to explore how addressing your gut brain connection and microbiome health could transform your weight loss journey.